In Brief
- Organ donation shortages are a critical issue around the world.
- 3-D bioprinting is a recent technology with great potential, particularly with the advancement of biomodeling.
- Ethical and legal considerations will need to accompany the progression of bioprinting techniques.
On average, 20 Americans die each day due to challenges surrounding organ availability. Around the world, people with the economic means will even buy organs off the black market. This global organ trade is a dangerous and illegal practice. However, science may come to the rescue. 3-D bioprinting is one of the latest cutting-edge technologies that can help organ supply meet demand. Bioprinting was launched in the late 1980’s using modified normal printers filled with “bioink,” a liquid mixture of cells and nutrients instead of traditional ink. Bioprinting soon gained 3-D capabilities and is slowly progressing from the experimental phase to clinical applications.
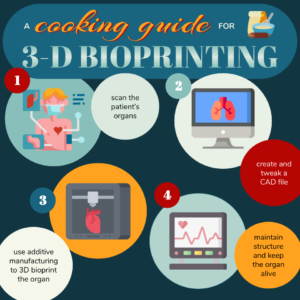
How 3-D Bioprinting Works: “A Cooking Guide”
Just as a chef can make a world-class dish tailored to customer wishes, those who operate bioprinters must cater their “bio-recipes” to each individual patient. Here’s the process:
- What better way to start than scanning the patient’s own organs and tissues? Typically, medical imaging techniques, such as computed tomography (CT) and magnetic resonance imaging (MRI) visualize objects. In CT, an X-ray source rotates around an item, where a sensor measures the beam intensity to draw a picture. In comparison, MRIs utilize strong magnetic fields to change the energy states of atoms within tissues, which characterize that shape. These initial bio-recipes are computer-aided design (CAD) files that help physicians determine the shape of the printed organ.
- Just as a chef might tweak a recipe, these files might also require tweaking to make them suitable for 3-D printing. After the CAD file is adjusted, it is converted into a format the bioprinter can understand, making the bio-recipe ready for production.
- On to the cooking! 3-D bioprinting works via a process called additive manufacturing. This methodology adds thin layers to a base until an object is created, similar to making a layer cake. The layers are composed of pluripotent stem cells derived from the patient’s own body. Since the cells are specific to the patient, this technique overcomes the problem of organ rejection.
- Now for the final touches. After printing, both mechanical and chemical stimulations are required to mature tissues and maintain their structural integrity, just as a world-class chef must perfect the structure and design of a dish. In bioprinting, this tricky step is not yet mastered, as it’s difficult to maintain the cells’ structure and keep them alive for long periods of time.
Design Issues & Potential Solutions
Sometimes, a direct copy of the patient’s organs may not be desirable due to injury or disease, thereby requiring changes to the design. Since physicians often must manually manipulate these scans, medical imaging alone is not a feasible approach for the mass production of bio-objects. A promising alternative method is biomodeling, which uses mathematical modeling techniques to either supplement or entirely replace medical imaging.
Current MRI and CT technologies are limited in their abilities to provide the highly detailed information required to accurately print at the cellular level, resulting in potential mechanical and structural issues in the tissue. Utilizing biomodeling techniques reduces this barrier by producing high-definition bio-recipes suitable for bioprinters. A group of scientists from universities in Turkey tackled this challenge of printing hollow structures using biomodeling to print an aorta. Remarkably, biomodeling aided in designing the aorta, resulting in a self-supporting structure that did not require a scaffold to maintain mechanical integrity. After obtaining a 3-D image of an aorta using traditional MRI and CT techniques, the team of researchers converted non-smooth scans into smooth surfaces suitable for 3-D printing using a simple algorithm.
Ethical Considerations and Future Directions
3-D bioprinting is a technology that is still in its infancy, and specific regulations are not yet developed in this field. One regulation needed in the future is identifying who is liable if the bioprinted organ malfunctions. “The complication is that there are many actors involved, from scientists, to companies, to doctors and health care system[s], patient[s], insurance etc., so there is no straightforward way to determine responsibility,’’ remarked Dr. Niki Vermeulen, a senior lecturer of History/Sociology of Science at the University of Edinburgh.
Moreover, the categorization of bio-objects — such as bioprinted organs — is a tricky issue, as they blur the line between non-life and life. In 2007, Dr. Vermeulen cofounded a network of researchers to reflect on recent developments in biotechnology and create a legal framework. This network gave rise to “Bio-objects and their Boundaries,” which continues discussion regarding bio-objects. The framework initially established can be applied to bioprinting.
More research is needed before the use of 3-D bioprinting becomes commonplace in precision medicine, specifically for organ transplants. The durability of bio-objects is still a mystery, but animal models may provide the key. Just as drug therapies are tested in animals before human use, bio-objects require further testing before they are ready for commercialization. However, the personalized nature of bio-objects “means that the normal safety and regulation paradigms do not work, and the patient treated with the first 3-D bioprinted organ transplant would be the proof person,” remarked Dr. Vermeulen. Regardless, 3-D bioprinting carries immense promise for biomedical advancement. It can potentially address organ shortages and save countless lives.
Content Expert
Dr. Niki Vermeulen is a senior lecturer of History/Sociology of Science at the University of Edinburgh. Her non-academic experience includes being a policy advisor and consultant in science and innovation policy for Technopolis, the Executive Board of Maastricht University and the Netherlands Scientific Council for Government Policy (WRR). She co-founded “Bio-objects and their Boundaries”, which includes members from 21 countries.
Works Cited
- Abouna, G. (2008). Organ Shortage Crisis: Problems and Possible Solutions. Transplantation Proceedings, 40(1), 34-38. doi:10.1016/j.transproceed.2007.11.067
- Bio-Objects. Retrieved from https://www.univie.ac.at/bio-objects/bioobjects.htm .
- Constructing ‘real’ Biological Structures Using 3D Bioprinting. (n.d.). Retrieved from https://www.scientificeuropean.co.uk/constructing-real-biological-structures-using-3d-bioprinting
- Kucukgul, C., Ozler, S. B., Inci, I., Karakas, E., Irmak, S., Gozuacik, D., . . . Koc, B. (2015). 3D bioprinting of biomimetic aortic vascular constructs with self-supporting cells. Biotechnology and Bioengineering, 112(4), 811-821. doi:10.1002/bit.25493
- Murphy, S. V., & Atala, A. (2014). 3D bioprinting of tissues and organs. Nature Biotechnology, 32(8), 773-785. doi:10.1038/nbt.2958
- Vermeulen, N., Haddow, G., Seymour, T., Faulkner-Jones, A., & Shu, W. (2017). 3D bioprint me: a socioethical view of bioprinting human organs and tissues. Journal of Medical Ethics, 43(9), 618–624. doi: 10.1136/medethics-2015-103347
- Organ Donation Statistics. (2019, March 08). Retrieved from https://www.organdonor.gov/statistics-stories/statistics.html#glance
- Rezende, R. A., Kasyanov, V., Mironov, V., & Silva, J. V. (2015). Organ Printing as an Information Technology. Procedia Engineering, 110, 151-158. doi:10.1016/j.proeng.2015.07.023
Image Credits:
Story Image: Aparna Kumar
Chief Editor: Sophie Zhang
Team Editor: Mary Chen
Team Graphic Designer: Aparna Kumar
This article was written by Hamza Alsamraee. Hamza and the cSw student editing team would like to thank Dani Gordon for serving as a mentor on this story. Dani is a Science/Technical writer at UT Health San Antonio
As always, before leaving a response to this article please view our Rules of Conduct. Thanks! -cSw Editorial Staff