Here’s a sobering statistic: 40% of Americans will be diagnosed with cancer at some point in their lifetimes. The statistic is even graver in the United Kingdom, where studies estimate that half the population will develop cancer in the future. Science is now catching up, however. Ever since President Richard Nixon declared war on cancer and signed the National Cancer Act in 1971, the world has seen major oncological breakthroughs. One of these notable advances is immunotherapy.
Since the 1940s, the primary strategy for treating cancer has been through the use of chemotherapy and radiation, along with the surgical removal of tumors when possible. However, immunotherapy, which may be more effective, is quickly becoming a reality. While its progress is slowed by certain obstacles, immunotherapy shows potential as an anti-cancer regimen.
Immunotherapy reinforces and strengthens the immune system to allow it to eradicate tumors, without the need for surgical or radiological intervention. It may surprise you to learn that small cancers develop in the body regularly. The reason we don’t notice is because our immune system is constantly fighting these cancers off and destroying them. However, every now and then, cancer cells begin to divide and grow at a rate that overwhelms the immune system. This is what leads to the disease. Strengthening the immune system presents an ingenious, almost obvious solution.
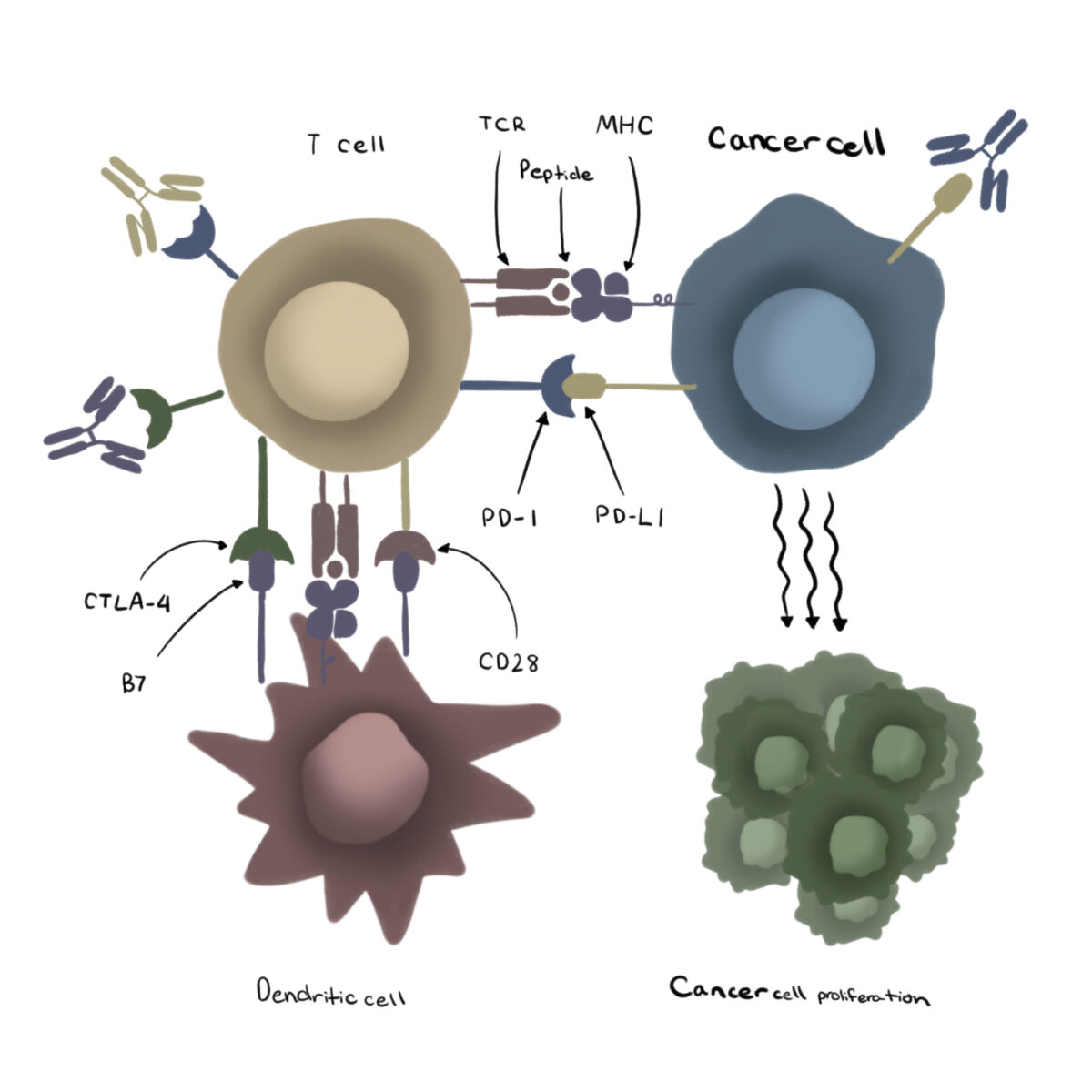
Immunotherapy encompasses a variety of treatments. One important kind of therapy is called ‘Immune Checkpoint Inhibition’ (ICI). Certain proteins in our immune system serve as ‘checkpoints’. These checkpoints regulate the immune response and prevent overactivity of the immune system. Cancer immunity is also controlled in this manner by certain cells in the bloodstream known as T-lymphocytes. ICI involves the injection of immunotherapeutic drugs (‘immune checkpoint inhibitors’) into the body to target and ‘inhibit’ these immune checkpoints. The blocking of these pathways in patients allows the immune system to respond much more vigorously to cancers than before. This method has shown significant improvements in patients with advanced cancers.
Dr Lalit Kumar, former Head of Medical Oncology at the All India Institute of Medical Sciences, New Delhi, believes that the introduction of immune checkpoint inhibition in the treatment of advanced cancers “has rapidly transformed the practice of oncology.”
Immunotherapy treatments are a cutting-edge advancement in medicine. Unfortunately, this means the drugs are often expensive and not accessible to all. Doctors in India recently found a possible solution.
In a study published in 2022 in the Journal of Clinical Oncology, researchers proved that low doses of nivolumab, an immune checkpoint inhibitor, showed significant benefits to patients with head and neck cancers.
The patients recruited for the study were randomly assigned to two groups. One group received the standard drug regimen for head and neck cancers. The other received the standard regimen in addition to ultra-low doses of nivolumab, an immune checkpoint inhibitor. These patients were given less than a tenth of what is considered the normal dose of the drug in the United States and Europe. After a year, the survival rate in the second group was almost three times higher than that of the first group. This highlights the profound benefits that even low doses of immunotherapeutic drugs can have on cancer treatment. This will greatly aid in cost management and making the treatment more accessible.
Another benefit of immunotherapeutic treatments is that their side effects are less severe than the alternatives to fighting cancer. While patients may experience diarrhea, skin rashes and muscle or joint pains, they avoid harsher side effects like alopecia (hair-loss) and vomiting, which are common in traditional chemotherapy. In very rare cases, immunotherapy drugs could cause autoimmune responses which target the lungs, intestines, liver, pituitary gland and kidneys.
While the first immunotherapeutic agent was approved by the FDA in 1986, progress in the field was initially slow. Like all medications, immunotherapeutic drugs required extensive testing on animal models, before they could be used by humans and brought to market. Common animal models include mice, rats and monkeys.
Cancer research often involves artificially introducing tumors into the bodies of these animals. This process involves weakening their immune systems in order to fuel cancer growth and prevent the immune system from interfering.
But this presents a tricky situation. In order to test immunotherapeutic drugs, the models must have uncompromised immune systems. Otherwise, assessing the efficacy of the medicines would be near impossible. This immunity suppression, which is required for cancer growth, hinders our ability to test medicines which act on the immune system.
Fortunately, technological advancements have helped scientists overcome this. For example, researchers have genetically engineered mice with alterations that facilitate cancer growth in specific tissues, so the defense systems of the models aren’t compromised.
Immunotherapy treatments are becoming increasingly available to more and more patients. Initially, immunotherapeutic agents were only administered to patients with advanced cancers or those who had previously failed rounds of chemotherapy and radiation.
“Current studies are exploring their application in early stages, sequence (in conjunction with chemotherapy), dosing schedule, and unraveling the mechanisms of resistance,”, says Dr Kumar.
Methods by which we can combine immunotherapies with chemotherapy and radiation are also under investigation. This research may signal a new frontier in the war on cancer. It holds the potential to loosen cancer’s grip on populations around the globe.
- Immunotherapy uses the body’s own immune system to fight cancer.
- Immune Checkpoint Inhibitors (ICI) are powerful cancer fighting drugs even at low doses.
- New mouse models are helping scientists study immunotherapeutic approaches.
Sources
- “Cancer Statistics,” National Cancer Institute. https://www.cancer.gov/about-cancer/understanding/statistics. Accessed August, 1, 2023
- Eno, Jessica. “Immunotherapy Through the Years,” J Adv Pract Oncol. 2017 Nov-Dec; 8(7): 747–753.
- Interview with Dr Lalit Kumar, former Head of Medical Oncology, All India Institute of Medical Sciences (AIIMS), New Delhi. Interview by Vinayak Talwar on July 23 2023.
- Jaber, Nadia. “Study in India Could Make Immunotherapy More Affordable Worldwide” 2022 November, National Cancer Institute. https://www.cancer.gov/news-events/cancer-currents-blog/2022/cancer-immunotherapy-low-dose. Accessed August 1, 2023.
- Olson, Brian et al. “Mouse Models for Cancer Immunotherapy Research,” Cancer Discov. 2018 Nov; 8(11): 1358–1365.
- Patil, Vijay Maruti, et al. “Low-Dose Immunotherapy in Head and Neck Cancer: A Randomized Study,” Journal of Clinical Oncology 41, no. 2 (January 10, 2023) 222-232.
- Torjesen, Ingrid. “Half of the UK population can expect a diagnosis of cancer,” BMJ 2015;350:h614
- Surh, Young-Joon. “The 50-Year War on Cancer Revisited: Should We Continue to Fight the Enemy Within?” J Cancer Prev. 2021 Dec 30; 26(4): 219–223.
Editorial Team
- Chief Editor: Annika Singh
- Team Editor: Tara Prakash
- Image Credit: Sylvia Xu
- Social Media Lead: Chloe Eng
Mentor
- Paula Clifford is the executive director for Americans for Medical Progress (AMP), a non-profit organization that provides innovative programs to provide information to the public about biomedical research and the important role animals have in advancing medicine and science.
Content Expert
Dr. Lalit Kumar is the former Head of Medical Oncology at All India Institute of Medical Sciences (AIIMS) in New Delhi. India.
