In Brief:
- Usher syndrome causes hearing loss and blindness and has no treatment
- Doctors at Boston Children’s Hospital have explored a mutation in the USH1C gene by replacing the defective gene with a functional gene in mice
- Treated mice hear noises at a much lower decibel than untreated mice
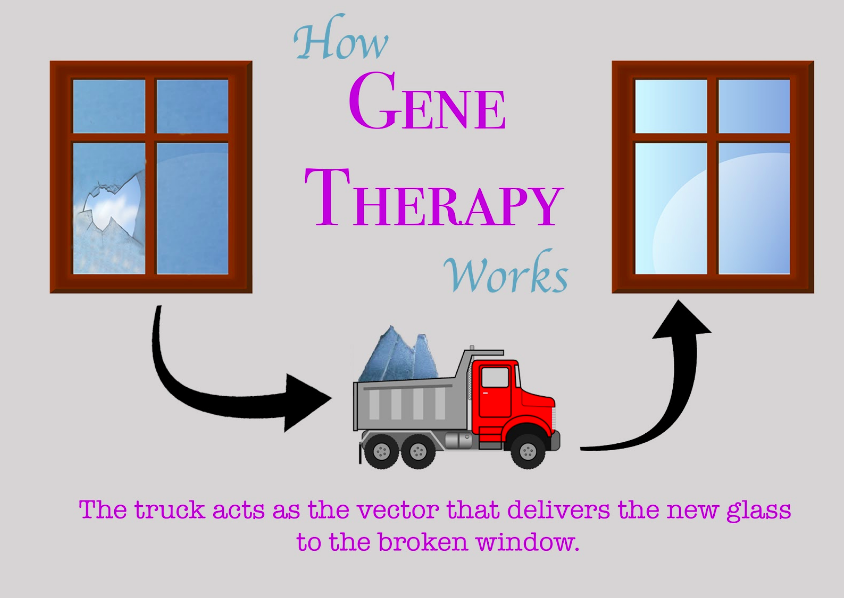
A baseball hits your window and leaves behind a large crack.
What’s the best way to solve this problem? A new Plexiglas® window would probably be the most effective long-term solution by ensuring a high quality, likely more resilient fix. So, you call a window replacement company that arrives at your house with a truck carrying materials. The new window is installed, and the window’s function is restored.
This process is similar to how gene therapy in humans works. The cracked window is like a defective gene. A vector, which is typically a virus that’s been modified to prevent it from causing disease, acts as the “truck” to deliver a corrected gene into the target tissue. Now, the corrected gene can give instructions to make important proteins that keep us healthy.
Dr. Gwenaelle Géléoc of the Department of Otolaryngology and F.M. Kirby Neurobiology Center at Boston Children’s Hospital has explored the use of gene therapy in treating Usher syndrome. Usher syndrome, the most common cause of deaf-blindness, is a genetic disorder that can cause loss of balance. Without a sense of balance and the ability to see and hear, many Usher syndrome patients live in an isolated world.
Dr. Géléoc and a team of researchers studied the effect of a specific gene, called the USH1C gene, in a model of Usher syndrome in mice. USH1C gives instructions to make a protein called harmonin, which Dr. Géléoc describes as “the nucleus of the Usher group of proteins.” Harmonin helps hair cells in the cochlea, a spiral structure in the inner ear, convert sound into electrical signals. Outer hair cells in the inner ear first amplify sound waves, and inner hair cells use the amplified vibrations to send messages to the brain. Mutations in the protein harmonin prevent proper growth of hair cells and lead to genetic deafness.
Researchers used a synthetic vector to deliver the corrected USH1C gene into the inner ear. To determine if treatment restored hearing, researchers measured activity in the auditory, that is, hearing related, regions of the mice brains after applying sounds of varying decibels. Normal mice detected sound in the 20-decibel range, while no electrical response was observed in genetically deaf mice at 110 decibel tones. Treated mice could detect sounds as low as 30 decibels, which can be compared to a whisper.
“This was basically the auditory sensitivity a normal mouse would have. The first time we saw this, I actually did not believe it because it was almost too beautiful to be true,” says Dr. Géléoc. “I really was skeptical, but we did it again and confirmed that we indeed were getting good recovery. So that was an ‘oh my gosh’ moment.”
However, Dr. Géléoc hesitates when asked about applying her research to human clinical trials. She stresses the need to conduct tests on larger animal models such as non-human primates or pigs before moving on to people.
The promise gene therapy brings is not without important obstacles. In 1999, 18-year-old Jesse Gelsinger was injected with a vector during a gene therapy clinical trial at the University of Pennsylvania. His immune system interpreted the virus as a foreign invader and attacked, leading to the first publicly identified death caused by gene therapy. The famous Gelsinger case tainted the public’s view of the technology and raised questions concerning safety.
Dr. Géléoc believes another significant hurdle is the cost of gene therapy. Gene therapy is individualized, which means each genetic mutation is treated differently. It will be very expensive to design a unique treatment for every patient.
An alternative for Usher syndrome patients is cochlear implants. A cochlear implant is an electronic device that is surgically placed into a patient’s cochlea to improve hearing. With this technology available, why are researchers like Dr. Géléoc so devoted to working with gene therapy? Why invest so much time and research into a costly technique still in need of improvement?
Cochlear implants are like placing tape over the crack in our window. They work, but it’s just not the same as before. Dr. Géléoc says, “When you talk to patients, they always say, ‘Cochlear implants are great, but I can’t really appreciate music like you do. And if too many people talk, I can’t follow conversations. We need you to do better than what we have available right now.’”
Dr. Géléoc listens to these concerns and works tirelessly to advance progress in Usher syndrome. Patients, once isolated in darkness, may soon experience the outside world through a “window” designed by thousands of scientists and strengthened by decades of research.
Plexiglas® is a registered trademark of Evonik Röhm GmbH, Darmstadt, Germany.
CONTENT EXPERT
Dr. Gwenaelle Géléoc is a Research Associate in Otolaryngology and Neurobiology at Boston Children’s Hospital and Assistant Professor of Otolaryngology at Harvard Medical School. As a principal investigator of the Holt/Géléoc Lab, which she runs with her husband, she conducts research involving the structure and function of sensory hair cells in the inner ear. When she is not busy working in the lab or writing articles, Dr. Géléoc enjoys running and spending time with her two children.
Works Cited
- Day, Suzanne. “Inside the Holt/Géléoc Lab.” Massachusetts Eye and Ear. Last modified September 1, 2014. https://www.masseyeandear.org/news/press-releases/2014/09/holt-geleo-lab-feature
- Géléoc, Gwenaelle. “USH Talks: Gene Therapy for Usher Syndrome Type 1C.” Presentation at USH Talks, February 6, 2017.
https://www.usher-syndrome.org/what-is-usher-syndrome/presentations/ush-talks/ush-talks-gene-therapy-for-usher-syndrome-type-1c.html - “Gene therapy restores hearing in deaf mice… down to a whisper.” Harvard Stem Cell Institute. Last modified March 27, 2017. https://hsci.harvard.edu/news/gene-therapy-restores-hearing-deaf-mice-down-whisper
- Interview with Dr. Gwenaelle Géléoc. Interview by Sophie Zhang. August 7, 2017
- Mathur, Pranav and Jun Yang. “Usher syndrome: Hearing loss, retinal degeneration and associated abnormalities.” Biochimica et Biophysica Acta 1852, no. 3 (March 2015): 406-420
- “What Is Usher Syndrome?.” NIDCD. Last modified March 6, 2017. https://www.nhlbi.nih.gov/health/health-topics/topics/hemophilia/
Image Credits:
Feature Image:
- [“Baseball” by Anonymous (Edited). License: CCO 1.0]
- [“DNA, Biology, Medicine, Gene” by PublicDomainPictures (Edited). License: CCO 1.0]
Story Image:
-
- [“Window, Window To The World, Pane, View, House” by kmicican (Edited). License: CCO 1.0]
- [“Truck Vector Clipart” by Steam Coded (Edited). License: CCO 1.0]
- [“Curved Arrow” by Amada44 (Edited). License: CCO 1.0]
- [“Broken Window, Hole, Glass, Damage, Shattered, Sharp” by skeeze (Edited). License: CCO 1.0]
- [“Broken Glass Shards Urban Exploration” by Steven Depolo (Edited). License: CCO 2.0]
Chief Editor: Aparna Ragupathi
Creative Team Manager: Sreya Das
Team Editor: Akansha Khurana
Team Graphic Designer: Riley Doyle
This article was written by Sophie Zhang. As always, before leaving a response to this article please view our Rules of Conduct. Thanks! -cSw Editorial Staff